Moving for Macular Health: How Physical Activity Supports Eyes with AMD
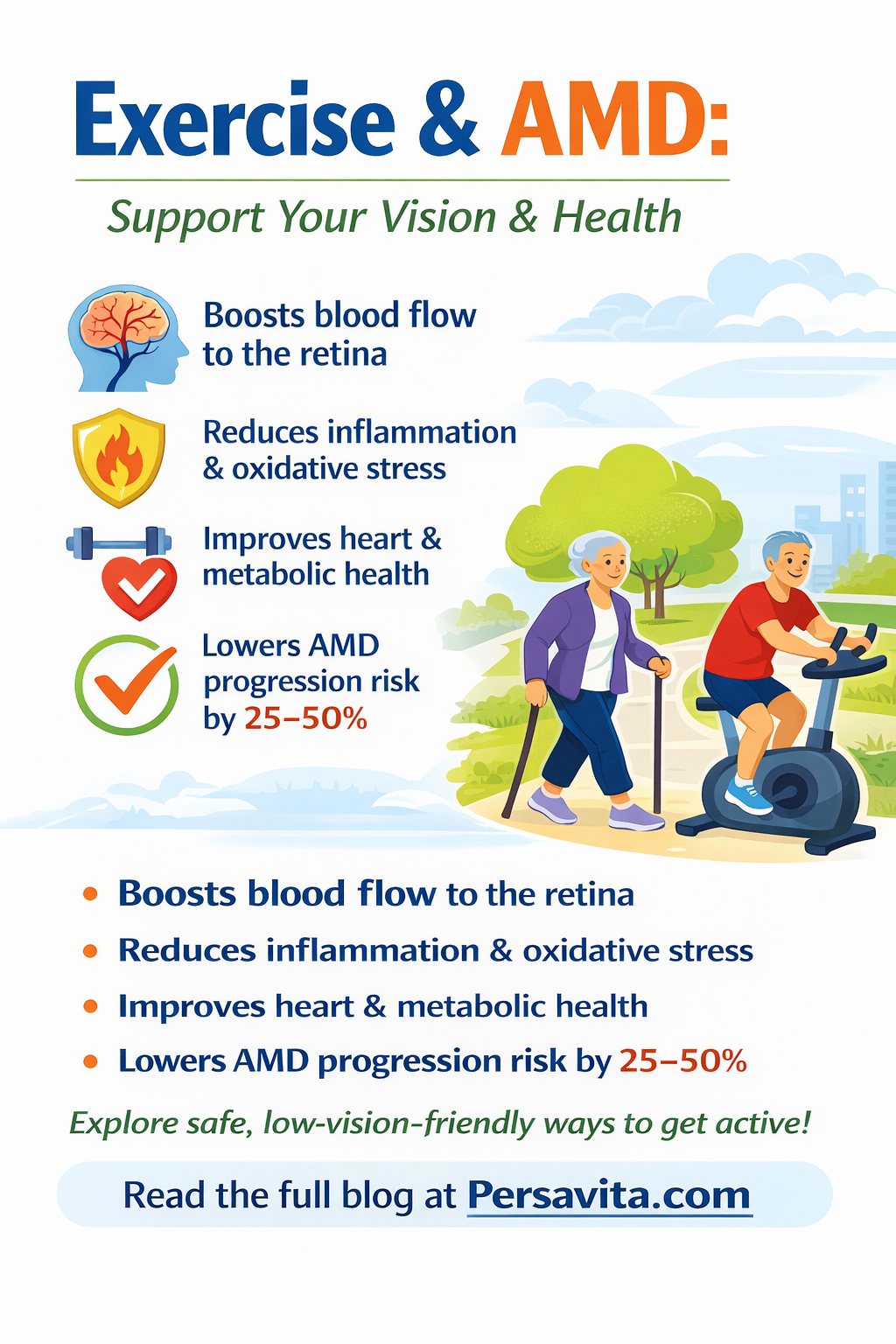
Staying active is one of the most powerful lifestyle steps people with age‑related macular degeneration (AMD) can take to protect both their vision and overall health. Regular movement supports blood flow to the retina, lowers inflammation, and improves heart and metabolic health—key factors linked to AMD risk and progression. Yet surveys show many AMD patients are unsure what kind of exercise is safe or useful for their eyes.How-well-do-patients-understand-exercise-effects-o.pdfpmc.ncbi.nlm.nih
Important: Always discuss any change in your physical activity with your ophthalmologist, family doctor, or other healthcare professional before you begin.
Why Exercise Matters for People with AMD
Large population studies have found that people who are physically active are less likely to develop AMD or progress to late stages of the disease. In some cohorts, those doing regular moderate‑to‑vigorous activity had 25–50% lower odds of early or late AMD compared with sedentary adults.pubmed.ncbi.nlm.nihHow-well-do-patients-understand-exercise-effects-o.pdf
Researchers think several mechanisms may explain this protective effect:
- Exercise improves cardiovascular fitness and blood flow, including to the tiny blood vessels that nourish the retina.pmc.ncbi.nlm.nih+1
- Physical activity reduces chronic inflammation and oxidative stress, two processes that damage macular cells over time.pmc.ncbi.nlm.nihHow-well-do-patients-understand-exercise-effects-o.pdf
- Active people tend to have better blood‑pressure, blood‑sugar, and weight control, all of which are linked with AMD outcomes.pmc.ncbi.nlm.nih+1
For many patients, clinicians emphasize diet and supplements but give little concrete guidance on movement. Surveys show exercise is often the least remembered lifestyle recommendation among AMD patients, despite this growing evidence base.Surveys-on-AMD-patient-knowledge-of-lifestyle-inte.pdf+1
How Much Activity Do AMD Patients Need?
Most people with AMD can safely follow the same evidence‑based activity targets recommended for older adults, with individual adaptations for vision and other health conditions.cdc+2
Aerobic (Endurance) Activity
Health agencies recommend at least 150–300 minutes per week of moderate‑intensity aerobic activity, such as brisk walking, comfortable cycling, or water aerobics. This could look like:health+2
- 30 minutes of walking, 5 days per week, or
- Several shorter 10–15‑minute walks spread across the day.
For those who are already fit and have medical clearance, 75–150 minutes of vigorous activity (for example, faster walking uphill or more intense cycling) can provide similar benefits in less time.heart+1
Strength (Resistance) Training
At least two days per week, adults should perform muscle‑strengthening activities that work the major muscle groups: legs, hips, back, abdomen, chest, shoulders, and arms. Examples include:cdc+1
- Sit‑to‑stand repetitions from a stable chair.
- Light dumbbells or resistance bands.
- Supervised gym or physiotherapy programs tailored to balance or joint limitations.
Maintaining muscle strength is essential for independence, fall prevention, and the ability to stay active despite visual changes.What-educational-materials-improve-exercise-adhere.pdfpmc.ncbi.nlm.nih
Balance and Flexibility
Because AMD can affect depth perception and confidence in new environments, balance‑focused exercises are especially important. Helpful options include:pmc.ncbi.nlm.nihWhat-educational-materials-improve-exercise-adhere.pdf
- Tai chi or gentle yoga designed for older adults.
- Heel‑to‑toe walking along a counter or rail.
- Standing on one leg while holding onto a sturdy surface.
These activities can be done 2–3 times per week and are often included in low‑vision rehabilitation or community fall‑prevention programs.pmc.ncbi.nlm.nih
Reducing Sitting Time
Even if weekly exercise goals are met, long, uninterrupted periods of sitting carry health risks. Guidelines suggest breaking up sitting every 30–60 minutes with a few minutes of light movement such as standing, stretching, or a short walk around the room.health+1
For AMD patients who use a lifestyle or “health score” system, realistic starting thresholds might be:
- Baseline: 5,000–6,000 steps per day or equivalent movement on most days.pmc.ncbi.nlm.nihHow-well-do-patients-understand-exercise-effects-o.pd
- Optimal: Meeting or exceeding 150 minutes/week of moderate activity plus 2 days of strength work.
Safe, Vision‑Friendly Exercise Ideas
Many people with AMD also live with arthritis, heart disease, or balance problems. The key is choosing activities that feel safe, enjoyable, and easy to navigate with low vision.pmc.ncbi.nlm.nihWhat-educational-materials-improve-exercise-adhere.pdf
1. Guided or Indoor Walking
- Walk in familiar, well‑lit environments such as shopping malls, indoor corridors, or flat neighborhood routes.
- Use a cane, walking poles, or a companion if balance or confidence is an issue.
- Start with 10‑minute walks and build up gradually.mdfoundation+1
2. Stationary Cycling
A stationary or recumbent bike lets patients get aerobic benefit without worrying about curbs, traffic, or uneven ground. Resistance—not speed—can be adjusted to match fitness and joint comfort.pmc.ncbi.nlm.nih+1
3. Water‑Based Exercise
Water walking, gentle swimming, and low‑impact aquatic classes reduce joint load while providing resistance for both strength and endurance. Pool lanes or instructor guidance can help with orientation if vision is limited.mdfoundation+1
4. Chair‑Based Routines
Chair‑based or supported standing programs are ideal for those with advanced AMD, severe joint disease, or high fall risk. They can include:
- Seated marching and leg raises.
- Resistance‑band exercises anchored under the feet or behind the chair.
- Gentle spinal and shoulder mobility work.What-educational-materials-improve-exercise-adhere.pdfpmc.ncbi.nlm.nih
These routines are frequently used in low‑vision and older‑adult rehabilitation programs and can be adapted for home with printed or audio‑described instructions.What-educational-materials-improve-exercise-adhere.pdfpmc.ncbi.nlm.nih
5. Mind‑Body and Relaxation‑Focused Movement
Tai chi, qigong, and similar practices combine slow, controlled movements with breathing and mental focus, which can improve balance, mood, and sleep—factors that strongly influence quality of life with AMD.pmc.ncbi.nlm.nihWhat-educational-materials-improve-exercise-adhere.pdf
Overcoming Common Barriers
Studies of AMD patients reveal recurring challenges: fear of falling, uncertainty about what is “safe,” low confidence, and a sense that exercise won’t specifically help their eyes.How-well-do-patients-understand-exercise-effects-o.pdf+1
Some practical strategies include:
- Link movement to what matters most. Explaining that walking or strength exercises support independence, driving, and time with grandchildren can make the benefits feel relevant, not abstract.ophthalmologyadvisorHow-well-do-patients-understand-exercise-effects-o.pdf
- Start small and build. Short, achievable goals (for example, “10 minutes of walking after lunch, 4 days this week”) are more sustainable than ambitious but unrealistic plans.How-well-do-patients-understand-exercise-effects-o.pdf+1
- Use prompts and tracking tools. Checklists, calendars, or digital apps that record daily steps or minutes help people see their progress and stay motivated over time.What-educational-materials-improve-exercise-adhere.pdfpmc.ncbi.nlm.nih
- Seek social support. Group classes, walking partners, or caregiver involvement often improve adherence and enjoyment.pmc.ncbi.nlm.nihWhat-educational-materials-improve-exercise-adhere.pdf
Clinicians and charities such as the Macular Society and Macular Disease Foundation offer accessible brochures and videos that show safe exercises step‑by‑step using large print and clear diagrams—resources that can be integrated into AMD coaching platforms.macular+1What-educational-materials-improve-exercise-adhere.pdf
When to Be Cautious and Seek Medical Advice
Exercise is not risk‑free, especially for adults with other medical conditions. Before starting or intensifying physical activity, AMD patients should talk with their healthcare team if they have:
- Heart disease, chest pain, or unexplained shortness of breath.
- Uncontrolled high blood pressure or diabetes.
- Recent eye surgery or new visual symptoms such as sudden distortion, flashes, or a dark curtain in vision.
- Severe joint pain, balance problems, or a history of frequent falls.
Clinicians can help tailor an activity plan, adjust medications if needed, and refer patients to physiotherapy or supervised programs when appropriate.cdc+1
Disclaimer
The content in this article is for general educational purposes only and is not intended as personal medical advice, diagnosis, or treatment. Any change in physical activity—especially if you have AMD, other eye disease, heart or lung problems, joint pain, balance issues, or chronic health conditions—must be discussed with and supervised by your ophthalmologist, family doctor, or another qualified healthcare professional. Never start, stop, or modify an exercise program based solely on information from this website.
References
- Choi JA et al. Physical activity, visual impairment, and eye disease. Ophthalmic Epidemiology. 2018. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC6085324/pmc.ncbi.nlm.nih
- Zhou X et al. Physical Activity and Age-related Macular Degeneration. 2017. PubMed: https://pubmed.ncbi.nlm.nih.gov/28549846/pubmed.ncbi.nlm.nih
- Macular Degeneration Research. Exercise Can Help Prevent or Slow Macular Degeneration. 2020. https://www.macular.org/care-and-treatment/reduce-your-risk/exercisemacular
- Macular Society. Exercise can slow or prevent vision loss, study finds. 2020. https://www.macularsociety.org/about/media/news/2020/july/exercise-can-slow-or-prevent-vision-loss-study-finds/macularsociety
- Lions Eye Institute. Exercise can slow or prevent macular degeneration. 2022. https://www.lei.org.au/about/news/exercise-can-slow-or-prevent-macular-degeneration/lei
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd edition. 2018. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdfhealth
- Centers for Disease Control and Prevention. Older Adult Activity: An Overview. 2025. https://www.cdc.gov/physical-activity-basics/guidelines/older-adults.htmlcdc
- Canadian Society for Exercise Physiology. 24‑Hour Movement Guidelines for Adults 65+. 2020. https://csepguidelines.ca/guidelines/adults-65/csepguidelines
- Macular Disease Foundation Australia. Exercise. 2024. https://www.mdfoundation.com.au/living-well/wellbeing/exercise/mdfoundation
- Levels of self‑reported and objective physical activity in individuals with AMD. Investigative Ophthalmology & Visual Science. 2020. https://pmc.ncbi.nlm.nih.gov/articles/PMC7372878/pmc.ncbi.nlm.nih
- Smith L et al. Physical activity interventions for adults who are visually impaired. Cochrane Review, 2020. https://pmc.ncbi.nlm.nih.gov/articles/PMC7045169/pmc.ncbi.nlm.nih
- “How well do patients understand exercise effects on macular health?” Evidence synthesis in: MacuGuard AMD Digital Nurse research pack.How-well-do-patients-understand-exercise-effects-o.pdf
- “What educational materials improve exercise adherence in AMD?” Evidence synthesis in: MacuGuard AMD Digital Nurse research pack.What-educational-materials-improve-exercise-adhere.pdf
- Targeting modifiable risk factors in age-related macular degeneration. Eye and Vision. 2017. https://pmc.ncbi.nlm.nih.gov/articles/PMC6095576/pmc.ncbi.nlm.nih
- Effects of lifestyle interventions to promote physical activity in older adults with chronic conditions. 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC12106156/pmc.ncbi.nlm.nih
- https://ppl-ai-file-upload.s3.amazonaws.com/web/direct-files/attachments/107425446/abc498b6-2598-4caf-b7b6-fc1a8831ad61/How-well-do-patients-understand-exercise-effects-o.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6085324/
- https://pubmed.ncbi.nlm.nih.gov/28549846/
- https://www.retinov.com/blog/physical-activity
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6095576/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12106156/
- https://ppl-ai-file-upload.s3.amazonaws.com/web/direct-files/attachments/107425446/5a6a5930-0707-4076-8f94-395e70425253/Surveys-on-AMD-patient-knowledge-of-lifestyle-inte.pdf
- https://www.cdc.gov/physical-activity-basics/guidelines/older-adults.html
- https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
- https://csepguidelines.ca/guidelines/adults-65/
- https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults
- https://ppl-ai-file-upload.s3.amazonaws.com/web/direct-files/attachments/107425446/723366b7-ac0c-4395-9d9d-5fc8d866b73c/What-educational-materials-improve-exercise-adhere.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7045169/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7372878/
- https://www.mdfoundation.com.au/living-well/wellbeing/exercise/
- https://www.ophthalmologyadvisor.com/features/impact-of-lifestyle-changes-for-age-related-macular-degeneration/
- https://www.macular.org/care-and-treatment/reduce-your-risk/exercise
- https://www.macularsociety.org/about/media/news/2020/july/exercise-can-slow-or-prevent-vision-loss-study-finds/
- https://www.lei.org.au/about/news/exercise-can-slow-or-prevent-macular-degeneration/

Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.