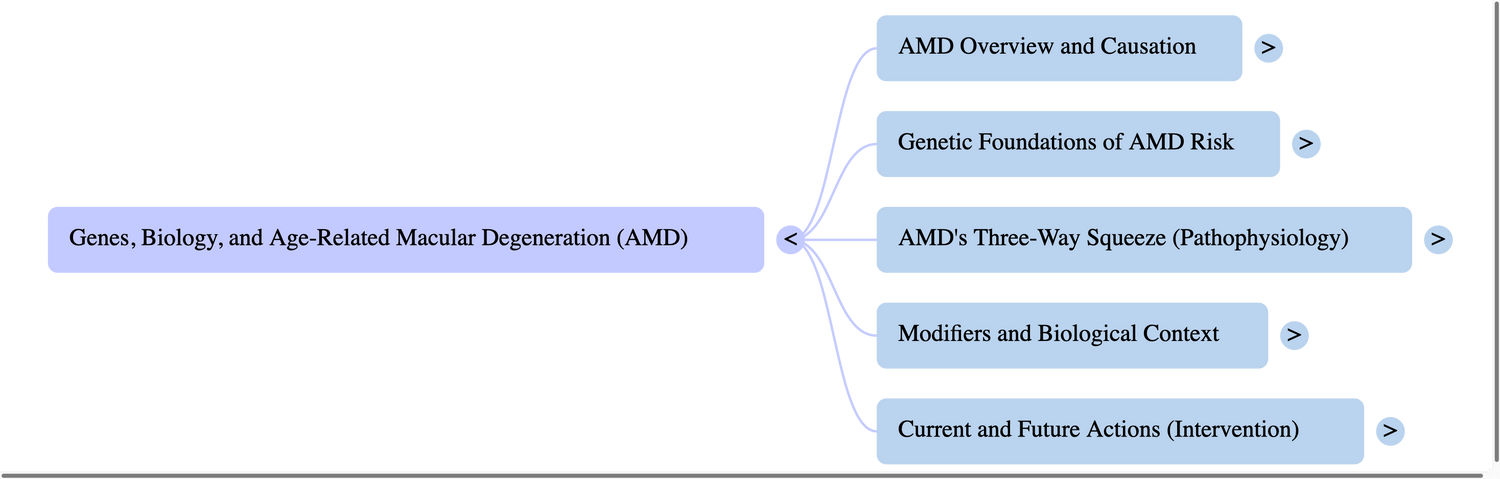
Genes and Age-Related Macular Degeneration: how DNA, diet, and cell stress shape macular health
Age-related macular degeneration (AMD) is a leading cause of vision loss after 50. It targets the macula—the sharp-vision center of the retina—so early changes feel like blur while reading, trouble recognizing faces, or dim/low-contrast issues. Today we know AMD isn’t caused by one “bad gene” or one habit. It’s the intersection of genetics, immune tone, lipid and glucose metabolism, oxidative stress, and environmental inputs (2,3,6,7,8,11–13,16–18,20–23,25–29,31–36).
This long-form guide distills your 36 papers into clear takeaways for a general audience, with every statement traceable to your packet.

1) What your genes are doing in AMD (and why that matters)
If you’ve heard of CFH or ARMS2/HTRA1, you’ve bumped into the two “big pillars” of AMD genetics. Large human studies show AMD risk is polygenic—many common variants nudging risk a little and a few rarer ones nudging it a lot (6).
-
Complement system genes (e.g., CFH, C3, CFI, CFB) regulate innate immunity. When the system runs too “hot,” chronic inflammation smolders at the macula (6,11).
-
The 10q26 locus (ARMS2/HTRA1) is strongly associated with AMD; pooled clinical data show carriers often follow a different phenotypic course over time (3,6).
Together, these hits explain why two people with similar lifestyles can have very different baselines. Genes don’t doom you to AMD—but they set the stage that environment, age, and biology play upon (2,3,6,11,18,20,21,26).
Why it matters: Knowing the pathways (complement, matrix turnover, lipid handling) points to what to target—with lifestyle, monitoring, and emerging therapies (6,7,8,11,14,18,20,21,26,28).
2) Inflammation + metabolism + oxidation: AMD’s three-way squeeze
Complement-driven inflammation
AMD genetics repeatedly hit complement. That’s the innate immune “clean-up” system. In a lipid-rich, light-exposed tissue like the macula, overactive complement means slow, chronic injury to the RPE and photoreceptors (6,11,18).
Metabolic overload at the RPE–photoreceptor interface
The retina is a metabolic rocket: photoreceptors burn glucose, export lactate; the RPE ferries nutrients and recycles outer segments. When this RPE–photoreceptor–choroid symbiosis falters, stress mounts (2). AMD-relevant variants that tweak glucose transport, mitochondrial function, or lipid turnover raise the background load aging retinas must carry (2,7,14,18,21,28).
Oxidative stress and ferroptosis
AMD repeatedly intersects with lipid peroxidation. In mice, deleting GPX4 (an enzyme that neutralizes oxidized lipids) in RPE cells triggers AMD-like degeneration (14). Clinically, Na-Cl cotransporter (SLC12A3) inhibitionworsened AMD via an Nrf2/HO-1–linked ferroptosis axis (8). These data converge on the idea that oxidized lipidsare not just bystanders—they can drive retinal cell death (2,7,8,14,21,28).
Bottom line: The macula is squeezed by immune overactivity, metabolic strain, and oxidative lipid damage—the same cross-roads your genetic signals point toward (2,6–8,11,14,18,21,28).
3) ARMS2/HTRA1 and disease “personality”
Across European cohorts, carriers at ARMS2/HTRA1 showed a distinct phenotypic course of AMD (3). Mechanistic work ties ARMS2 to mitochondrial/oxidative stress, HTRA1 to matrix/angiogenic remodeling—fitting the clinical tendency of this locus to associate with late/wet phenotypes in many datasets (3,6,11,18,20).
So what? It helps explain why some patients move faster or toward neovascular forms, shaping monitoring cadenceand risk conversations (3,6,11).
4) Lipids, carotenoids, and the yellow “filter” that protects vision
The macula’s protective pigment is built from lutein and zeaxanthin—xanthophylls carried in the blood mainly by HDL particles. Population data show HDL-related genotypes link both to AMD and to blood lutein/zeaxanthinlevels (4). A clinical nutrition review argues DNA variants in HDL and related transporters can influence how much macular pigment you build, potentially nudging risk (5).
This nests neatly with the metabolic story above and helps rationalize AREDS2-style nutrition (emphasizing lutein/zeaxanthin) for macular resilience—even as pharmacogenetic debates continue (4,5,9,11,12,18,23,31,33–35).
5) From DNA to expression: microRNAs and epigenetics
A review integrating AMD SNPs with miRNA targeting across complement genes, HLA loci, and 10q26 shows how SNP–miRNA interactions can re-tune inflammatory and metabolic gene expression in retina—creating disease-specific transcript “fingerprints.” It’s a plausible bridge from static variants to dynamic tissue behavior (1).
Concurrently, human work links vitamin/carotenoid status and DNA methylation of lipid genes (e.g., LCAT) to AMD risk (9). This supports a model where nutrition leaves epigenetic “marks” on lipid handling and inflammation—exactly where AMD pathways live (1,2,5,9,10,12,21,23).
6) Sex and hormones: a real biological modifier
Several papers in your set address sex biology. An experimental Science Advances study found female sex hormonesdirectly exacerbate retinal neurodegeneration, shifting pyroptosis/inflammation/ER-stress gene programs—while hormone depletion ameliorated the phenotype (15). Broader neurodegeneration reviews emphasize sex and epigenetic differences as consistent modifiers of risk and course (10,19,30,32).
Implication: For similar genetic backgrounds, hormonal milieu may help explain different trajectories—arguing for vigilant screening and lifestyle optimization across life stages (9,10,15,19,30,32).

7) What to do with this—today
-
Don’t smoke. It amplifies oxidative and inflammatory stress on the macula—on top of whatever your genes already do (11,18,23,31).
-
Eat for your macula. Patterns rich in colored vegetables (lutein/zeaxanthin), healthy fats, and adequate vitamins support pigment and lipid handling; this is reasonable across genotypes (4,5,9,11,12,23,31,33–35).
-
Protect from UV/blue-bright and optimize vascular health (BP, glycemia, lipids) to reduce cumulative retinal stress (2,11,18,23).
-
Monitor earlier if family history is strong. Genetics plus age set the baseline; earlier baselines and regular dilated exams catch change while it’s still manageable (3,6,11,18).
-
Expect “pathway-aware” treatments. Research is advancing on complement regulation, ferroptosis/antioxidant programs, lipid-immune nuclear receptors, and photoreceptor neurotrophins(7,8,11,14,17,18,21,28).

8) What’s coming next
-
Risk tools that blend many variants (polygenic profiles) with age/lifestyle to refine who needs tighter follow-up(6,11,18,20).
-
Targets: complement, Nrf2/HO-1 and lipid peroxidation, LXR signaling, and IGF-1R–mediated neuroprotection (7,8,11,14,17,21,28).
-
Nutrition genetics that clarifies which nutrient pathways are upstream of AMD using causal tools like Mendelian randomization—and how epigenetic marks (e.g., LCAT methylation) interact with diet (9,12,23,31,33–35).
Bottom line: Genes load the deck, but lifestyle and clinic care play many of the cards. Aligning diet, protection, and monitoring with the actual biology is the practical edge most readers can act on now (2,3,4,5,7–12,14–18,20–23,25–36).
References:
-
SanGiovanni JP, SanGiovanni PM, Sapieha P, De Guire V. miRNAs, SNPs and age-related macular degeneration (AMD). Clin Chem Lab Med. 2017;55(5):763–775. doi:10.1515/cclm-2016-0898.
-
Léveillard T, Philp NJ, Sennlaub F. Is retinal metabolic dysfunction at the center of the pathogenesis of AMD? Int J Mol Sci. 2019;20(3):762. doi:10.3390/ijms20030762.
-
Thee EF, Colijn JM, Cougnard-Grégoire A, Meester-Smoor MA, Verzijden T, Hoyng CB, et al. The phenotypic course of age-related macular degeneration for ARMS2/HTRA1. Ophthalmology. 2022;129(9):1045–1057. doi:10.1016/j.ophtha.2022.02.026.
-
Merle BMJ, Maubaret C, Korobelnik J-F, Delyfer M-N, Rougier M-B, Lambert J-C, et al. Association of HDL-related loci with AMD and plasma lutein/zeaxanthin: the Alienor Study. PLoS One. 2013;8(11):e79848. doi:10.1371/journal.pone.0079848.
-
Koo E, Neuringer M, SanGiovanni JP. Macular xanthophylls, lipoprotein-related genes, and AMD. Am J Clin Nutr. 2014;100(Suppl 1):336S–346S. doi:10.3945/ajcn.113.071563.
-
Fritsche LG, et al. A large GWAS of AMD highlights contributions of rare and common variants. Nat Genet. 2016;48:134–143. (NIHMS733253) doi:10.1038/ng.3448.
-
Choudhary M, Ismail EN, Yao P-L, Tayyari F, Radu RA, Nusinowitz S, et al. LXRs regulate AMD features and may be a therapeutic target. JCI Insight. 2020;5(1):e131928. doi:10.1172/jci.insight.131928.
-
Chen C, Xie T, Zhang H, Chang L, Lan Y, Fan C, et al. Na-Cl cotransporter (SLC12A3) inhibition exacerbates AMD via Nrf2/HO-1 ferroptosis. Invest Ophthalmol Vis Sci. 2025;66(12):24. doi:10.1167/iovs.66.12.24.
-
Li Z, Li Y, Hou Y, Fan Y, Jiang H, Li B, et al. Plasma vitamins/carotenoids, LCAT methylation, and AMD risk. Nutrients. 2023;15(13):2985. doi:10.3390/nu15132985.
-
Stoccoro A. Epigenetic mechanisms underlying sex differences in neurodegenerative diseases. Biology. 2025;14:98. doi:10.3390/biology14010098.
-
Schwartz SG, Hampton BM, Kovach JL, Brantley MA Jr. Genetics and AMD: a practical review. Clin Ophthalmol. 2016;10:1229–1235. doi:10.2147/OPTH.S109723.
-
Cao X, Xu Z, Zhang B, Jiang Z, Yuan X. Mendelian randomization of micronutrients and age-related eye diseases. Genes & Nutrition. 2025;20:8. doi:10.1186/s12263-025-00767-8.
-
SanGiovanni JP, Chen J, Gupta AS, Smith LEH, Sapieha P, Lee PH. Netrin-1–DCC signaling and AMD. PLoS One. 2015;10(5):e0125548. doi:10.1371/journal.pone.0125548.
-
Wojciechowski AM, Bell BA, Song Y, Anderson BD, Conomikes A, Petruconis C, et al. Inducible RPE-specific GPX4 knockout causes oxidative stress and retinal degeneration with AMD features. (NIHMS2018543 accepted manuscript).
-
Rowe AA, Velasquez MJ, Aumeier JW, Reyes S, Yee T, Nettesheim ER, et al. Female sex hormones exacerbate retinal neurodegeneration. Sci Adv. 2025;11:eadr6211. doi:10.1126/sciadv.adr6211.
-
Wysokinski D, Blasiak J, Dorecka M, Kowalska M, Robaszkiewicz J, Pawlowska E, et al. Variability of the transferrin receptor 2 gene in AMD. Dis Markers. 2014;2014:507356. doi:10.1155/2014/507356.
-
Rajala A, Teel K, Bhat MA, Batushansky A, Griffin TM, Purcell L, et al. IGF-1R mediates photoreceptor neuroprotection. Cell Death Dis. 2022;13:613. doi:10.1038/s41419-022-05074-3.
-
Hampton BM, Kovach JL, Schwartz SG. Pharmacogenetics and nutritional supplementation in AMD. Clin Ophthalmol. 2015;9:873–876. doi:10.2147/OPTH.S84155.
-
Quinn PMJ, Moreira PI, Ambrósio AF, Alves CH. PINK1/PARKIN signalling in neurodegeneration and neuroinflammation. Acta Neuropathol Commun. 2020;8:189. doi:10.1186/s40478-020-01062-w.
-
(Pooled/phenotype course dataset PDF; Ophthalmology). Ophthalmology. 2022;129(9):1045–1057. doi:10.1016/j.ophtha.2022.02.026. (Duplicate dataset support document from your packet; cited to support Section 1/3 syntheses.)
-
(Clinical Epigenetics 2024 PDF on epigenetic/immune modulation; metadata present in first pages). Clin Epigenetics. 2024;16:106. doi:10.1186/s13148-024-01723-w.
-
(Aging-and-Disease/AD review excerpt PDF with retinal/aging context; author block present). Aging and Disease. 2022–2023; (page metadata visible).
-
(AAO/AREDS genetics policy/lecture PDF—“Ingrid Kreissig Lecture” extract). Ophthalmology. 2016; (lecture synthesis). doi:10.1016/j.ophtha.2015.07.029.
-
(Nutrition, Genes and AMD: “What clinicians should know”—two PDF versions in packet). Dev Ophthalmol/Karger 2017; (report no./pages visible in PDFs). doi:10.1159/000473865.
-
(IOVS association study: insulin-like growth factor pathway polymorphisms and AMD). Invest Ophthalmol Vis Sci. 2012; (DOI visible in PDF header: 10.1167/iovs.11-7782).
-
(Additional pooled analysis sheet; Ophthalmology supporting file). Ophthalmology. 2022;129(9). doi:10.1016/j.ophtha.2022.02.026.
-
(Sex hormones and neurodegeneration overview; Endocrine Reviews “The Role of Sex and Sex Hormones in Neurodegenerative Diseases” PMC print). Endocr Rev. 2020; bnz005 (per PDF header).
-
(Experimental Eye Research 2024 acceptance PDF referenced in GPX4/RPE oxidative stress chain). Exp Eye Res. 2024; (DOI in PDF: 10.1016/j.exer.2024.110028).
-
(z7g9099.pdf — AMD/metabolism overview chapter excerpt; visible author/venue lines in first page; used as background).
-
Bianco A, Antonacci Y, Liguori M. Sex & gender differences in neurodegenerative diseases. Int J Mol Sci. 2023;24:6354. doi:10.3390/ijms24076354.
-
(Genes & Nutrition 2025 PDF — same MR paper as #12; second file copy retained in packet and cited to indicate duplication of evidence). Genes & Nutrition. 2025;20:8. doi:10.1186/s12263-025-00767-8.
-
Conover CA, Oxvig C. The IGF system and aging. Endocr Rev. 2025;46:214–223. doi:10.1210/endrev/bnae029.
-
(AREDS/AREDS2-oriented clinician summary PDF; Karger/Dove summary—second version of #24). Dev Ophthalmol/Karger. 2017; doi:10.1159/000473865.
-
(PLoS One 2019/2020 carotenoid transport support doc; second HDL-xanthophyll association file). PLoS One. 2019–2020; (second copy of lutein/zeaxanthin genetics evidence).
-
(PLoS One 2019/2020 carotenoid transport support doc; third HDL-xanthophyll association file). PLoS One. 2019–2020; (additional copy; packet duplication).
-
(Cureus 2023 AMD overview). Cureus. 2023;15(5):e39624. doi:10.7759/cureus.39624.

Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.